Temporomandibular joint disorders
Temporomandibular joint disorders (TMD)
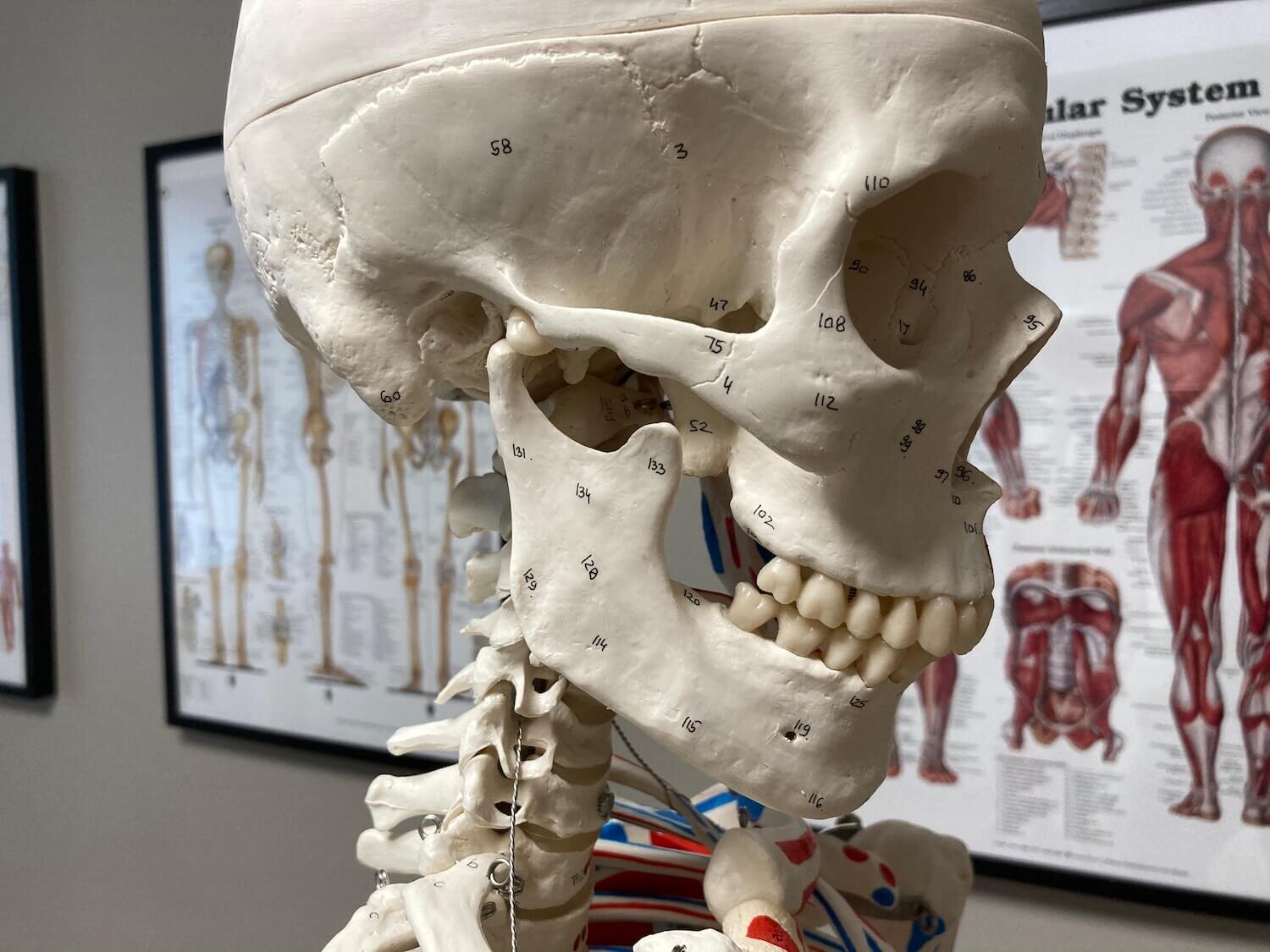
Stomatognatic system is an important anatomical system which comprises of the jaw including temporomandibular joints (TMJ), teeth and associated soft tissues. Its main functions include breathing, speaking and eating. Temporomandibular disorders are a term used for dysfunction. Dysfunctions of the stomatognatic system are commonly referred as temporomandibular disorders (TMD) which cover a variety of painful conditions, problems or dysfunctions arising from the temporomandibular joint, masticatory muscles or the surrounding tissues.
It is estimated that up to 50% of the population suffer from symptoms of TMD but only 10% of those seek professional help. Symptoms of temporomandibular disorder typically start between 20-50 years of age and the risk of having TMD is up to four times higher in women compared to men. TMD is typically divided into functional muscular cause and structural intra-articular cause or combinations of the two. However, the most common cause for dysfunction and pain is muscular from the muscles of mastication.
Common signs and symptoms
TMJ related sounds such as clicking and cracking
Pain, restricted movement and/or fatigue of the associated tissues
Headache and/or facial pain
Ear symptoms (e.g. pain or reduced hearing)
Throat symptoms (e.g. problem swallowing)
Pain or stiffness in the neck or shoulders
Dizziness
Common risk factors
Bruxism
Continuous jaw straining such as chewing gum or arm leaning (parafunctional activities)
Life dissatisfaction and negative psychological symptoms
Previous trauma to the jaw or neck
Female gender
Certain oral conditions such as open or cross bite
General joint hypermobility
Conservative management of TMD
Prior to care, it is very important to assess the nature and severity of the problem and identify all the risk factors for TMD. It has been shown that combination care is usually the most effective. Conservative treatment often includes reassurance, lifestyle and home advice to reduce gum chewing and arm leaning, as well as focusing on good sleep hygiene. If there are negative psychological aspects or somatisation the patient should be evaluated and possibly treated by a mental health professional. In acute cases short term NSAID’s and analgesics are often recommended which aim to reduce symptoms and provide temporary relief. Hot or cold therapy is also often recommended in the early stages of care. Occlusal therapy should be considered, if there is a history of bruxism, in order to reduce the muscular strain and dental abrasion.
Functional muscle related problems typically respond well to manual therapy. Chiropractors and other specialized manual therapists work to reduce the myofascial tightness which often help to alleviate the patient’s symptoms. Chiropractors also use hands on techniques such as stretching, trigger point therapy, joint mobilisation/manipulation and home exercises to restore normal TMJ movement and reduce the tension in the associated soft tissues and hopefully prevent the problem from reoccurring.
Sources:
Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain 1999;13:232-7
Okeson, J.P. (2013) Management of temporomandibular disorders and occlusion. [Text] 7th ed. St. Louis, Missouri, USA: Mosby Elsevier.
Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. Lippincott Williams & Wilkins; 2017 Sept 13.
National Institute for Health and Care Excellence, 2016. Temporomandibular disorders (TMDs) - NICE CKS [online]. Nice.org.uk. Available from: https://cks.nice.org.uk/ temporomandibular-disorders-tmds#!management [Accessed 30 Jul 2018].
Wright, E.F. (2014) Manual of temporomandibular disorders. 3rd ed. Chichester: Wiley Blackwell. [Electronic Book] Available at: https://aecc.idm.oclc.org/login?url=http:// lib.myilibrary.com?id= 553185(Accessed: 29 July 2018).
Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain 1999;13:232-7
Türp, J. C., Jokstad, A., Motschall, E., Schindler, H. J., Windecker-Gétaz, I., & Ettlin, D. A. (2007). Is there a superiority of multimodal as opposed to simple therapy in patients with temporomandibular disorders? A qualitative systematic review of the literature. Clinical oral implants research, 18 Suppl 3, 138–150. https://doi.org/10.1111/j.1600-0501.2007.01480.x